Existing Patients
(740) 344-4549
New Patients
(740) 212-1897
If a dentist recommends a root canal, it’s understandable to feel a little apprehensive — but there’s no need to panic. Modern root canal therapy is a precise, well-established treatment that removes the source of deep tooth pain and restores the function of a tooth that would otherwise be at risk. In many cases the experience is comparable to having a routine dental filling, with an emphasis on comfort and safety.
At the office of Brian Howe DDS, Family Dentistry, our team combines experienced clinical skill with modern instruments to make root canal treatment as predictable and comfortable as possible. We focus on clear explanations, gentle techniques, and individualized care so you understand your options and feel confident in your treatment plan.
When a tooth’s inner tissues are injured or infected, root canal therapy offers a reliable way to keep the natural tooth rather than extract it. Removing the damaged pulp, cleaning the internal canals, and sealing the tooth helps eliminate infection, stop pain, and restore chewing function. With appropriate restoration afterward, treated teeth often remain functional for many years.
Advances in endodontic instruments, imaging, and materials have improved both the comfort and long-term success of root canal treatments. Many teeth that would once have been removed can now be saved and restored to full function. Choosing to preserve a natural tooth when feasible helps maintain your bite, appearance, and oral health.
Deciding between extraction and root canal therapy involves several factors — the condition of the tooth, surrounding bone support, and the restoration required afterward. Our approach is conservative and evidence-based: when a root canal can reliably save your tooth, we present it as the preferred option because preserving your natural dentition supports better long-term outcomes.

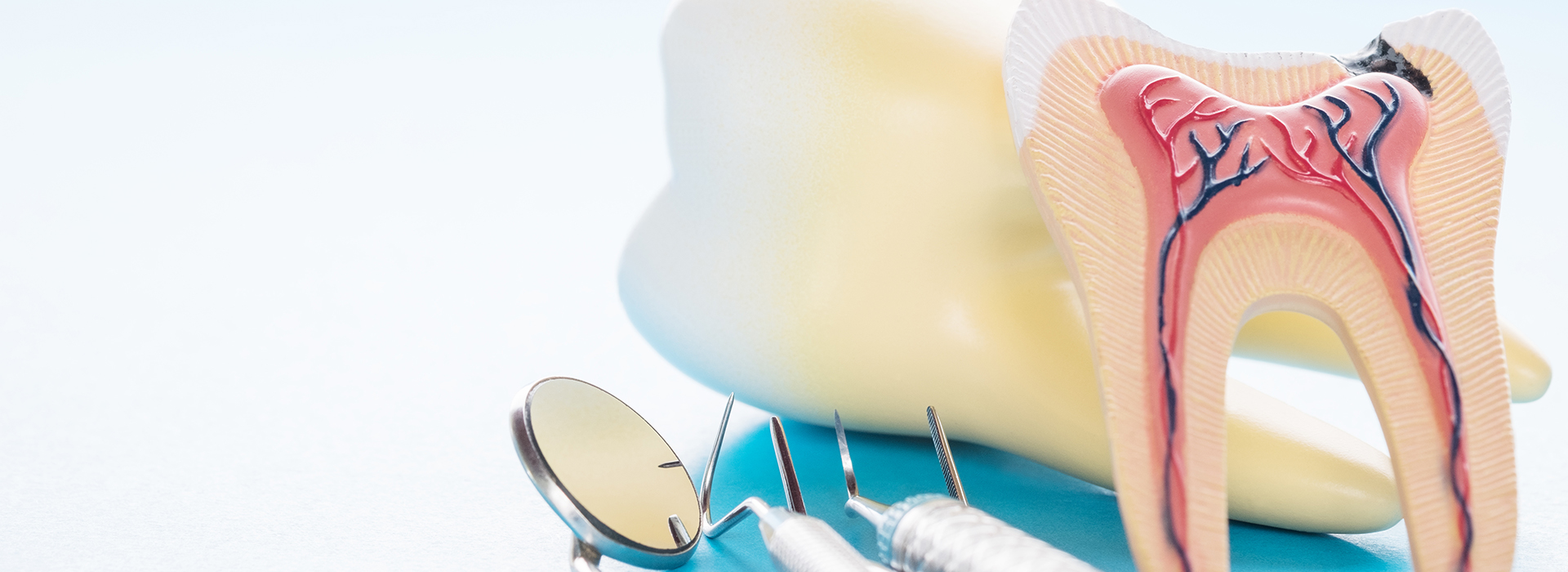
Teeth are more than their hard outer surfaces. Beneath the enamel and dentin lies the dental pulp — a soft tissue that contains nerves and blood vessels. When decay, trauma, or deep restorations reach this inner chamber, the pulp can become inflamed or infected. That internal irritation often produces noticeable symptoms that tell you and your dentist something needs attention.
Symptoms can vary from a nagging sensitivity to sharp, persistent pain. Some teeth announce trouble with heightened sensitivity to hot or cold, pain when biting, or spontaneous aching that interrupts sleep. Other issues, like discoloration or swelling, may indicate a longer-standing problem that requires treatment even if the pain is intermittent.
Because symptoms can overlap with other dental conditions, a careful exam and radiographs are essential for an accurate diagnosis. Detecting pulp involvement early gives you more options and increases the likelihood of saving the tooth with root canal therapy rather than facing extraction and replacement.
Although not every ache means a root canal is required, common warning signs to watch for include:
Pain that lingers or recurs despite home care often signals that the inner tissues of the tooth are affected. Toothaches that wake you at night or intensify with little provocation are classic indicators of significant irritation or infection and should be evaluated promptly.
If hot or cold foods cause an intense, lingering reaction, the nerve supply inside the tooth may be inflamed or damaged. While sensitivity can stem from many causes, extreme responses are a reason to seek a clinical assessment.
Discomfort when chewing or pressure-related pain often means the affected tooth’s structure or pulp is compromised. This type of pain can be sharp and localized, and it sometimes grows worse if left untreated.
A tooth that changes color after an injury or over time can be a sign that the internal tissues have deteriorated. Discoloration doesn’t always hurt, but it can indicate that the pulp is no longer healthy.
Trauma that breaches the protective layers of a tooth can expose the pulp to bacteria and infection. Even small fractures may allow irritants to reach the inner chamber and eventually necessitate root canal treatment to preserve the tooth.
Swelling around the gum or a visible bump on the gum surface can indicate an abscess — a localized infection that requires prompt attention. In some cases an abscess drains on its own, but professional treatment is still needed to eliminate the source and prevent recurrence.
Infections that affect the supporting bone or periodontal structures can produce mobility. Treating the infection inside the tooth and restoring it appropriately often helps resolve symptoms and stabilize the tooth as healing occurs.

Early evaluation matters. When irritation or infection is addressed promptly, treatment tends to be simpler, faster, and more successful. Delaying care can allow an infection to spread, damage surrounding structures, and reduce the options for preserving the tooth.
Radiographs and clinical testing often reveal problems before they cause extreme discomfort. A routine exam can uncover changes at the root tip or signs of chronic inflammation that you may not yet feel. By catching issues early, we can plan a conservative solution that preserves function and limits restorative work.
Acting early also reduces the risk of complications that can affect overall oral health. Removing an infected pulp and sealing the tooth removes the reservoir of bacteria, helps resolve associated bone inflammation, and prevents the infection from threatening neighboring teeth or tissue.
Root canal therapy is performed with local anesthesia to keep you comfortable throughout the procedure. We use refined instruments and magnification to access the tooth’s internal anatomy, carefully remove inflamed or infected tissue, and shape and clean the canal system before sealing it with a biocompatible material.
Some cases are completed in a single visit, while others call for two or more appointments depending on the tooth’s complexity and whether an active infection requires medication between visits. Throughout treatment we prioritize gentle technique and clear communication so you know what to expect at each step.
For patients who experience dental anxiety, sedation dentistry options are available to help you remain calm and relaxed during treatment. After the root canal, the tooth will typically need a permanent restoration such as a crown to restore strength and protect it from fracture — a key step in securing the long-term success of the therapy.

Following treatment it’s normal to experience mild soreness as the surrounding tissues heal. This usually subsides over a few days and can be managed with over-the-counter pain relievers as recommended. Our goal is to ensure your recovery is smooth and that you have clear instructions for home care.
At the office of Brian Howe DDS, Family Dentistry, we emphasize follow-up and the timely placement of a protective restoration. Leaving a treated tooth without a permanent crown or appropriate filling increases the risk of fracture. Restoring the tooth restores function and helps it endure the demands of everyday chewing.
With attentive home care and regular dental checkups, a properly treated and restored tooth can provide many years of reliable service. We’ll monitor healing with periodic radiographs and exams to confirm that the bone and surrounding tissues are responding well.
After your root canal procedure, you may experience the following:
You may feel numb for an hour or two after the appointment. During that period, avoid eating hot foods and be careful not to bite your lips, tongue, or cheek until normal sensation returns.
Some tenderness or mild soreness around the treated tooth is normal for a few days. The discomfort typically diminishes steadily; if it increases or fails to improve, contact the office so we can assess your healing.
If antibiotics are prescribed to manage an infection, take the full course exactly as directed. Stopping early can allow bacteria to persist and may complicate healing.
Until a permanent crown or restoration is placed, the tooth is more prone to damage. Avoid hard or sticky foods on that side and follow any temporary restoration care instructions we provide.
Continue brushing and flossing with care to support healing and overall oral health. Good home hygiene helps prevent new problems and supports long-term success.
Placing a permanent crown or suitable restoration is essential to strengthen the tooth and protect it from fracture. We will coordinate the restorative phase so you regain full function as soon as possible.
Root canal therapy is a proven way to relieve pain, stop infection, and preserve your natural tooth when the pulp is compromised. Our team combines experienced clinicians, modern technology, and a patient-centered approach to deliver care that prioritizes comfort and long-term results.
If you have questions about root canals or think you may need an evaluation, please contact us for more information. Our team is ready to help you understand your options and arrange timely care.
Root canal therapy treats the dental pulp, the soft tissue inside a tooth that contains nerves and blood vessels. When that pulp becomes inflamed or infected because of deep decay, trauma, or repeated dental work, the condition can cause persistent pain, sensitivity, or swelling and may threaten the tooth's survival. The primary goal of the procedure is to remove the diseased tissue, thoroughly clean the internal canal system, and seal the tooth to prevent further infection.
By eliminating the source of infection and sealing the space, root canal treatment relieves pain and preserves the natural tooth structure whenever possible. Preserving a natural tooth helps maintain proper chewing function, adjacent tooth position, and overall oral health. Early diagnosis and treatment increase the chances of a predictable, long-lasting result.
Symptoms that suggest pulp involvement include ongoing or severe toothache, heightened sensitivity to hot or cold that lingers, pain when biting, gum swelling or a pimple-like bump on the gum, and a tooth that darkens in color. Some cases produce intermittent discomfort or minimal symptoms while an infection progresses, so absence of severe pain does not always mean the tooth is healthy. A careful clinical exam and radiographs are necessary to confirm whether the pulp is inflamed or infected and to determine the extent of any damage.
Because several dental conditions can cause similar symptoms, your dentist will use tests such as percussion, bite evaluation, pulp vitality testing, and X-rays to make an accurate diagnosis. Catching problems early often allows for simpler treatment and better long-term outcomes. If you notice warning signs, scheduling an evaluation promptly preserves more options for saving the tooth.
Root canal therapy is performed under local anesthesia to ensure comfort throughout the procedure. The dentist creates an access opening, uses specialized instruments and magnification to remove inflamed or infected pulp, shapes and disinfects the canal system, and then fills and seals the canals with a biocompatible material. When necessary, a temporary restoration is placed until a permanent crown or filling is completed to protect the tooth from fracture.
Some teeth are treated in a single visit while others require two or more appointments when active infection or complex anatomy is present. At the office of Brian Howe DDS, Family Dentistry, we combine modern endodontic instruments, imaging, and gentle techniques to make the process predictable and as comfortable as possible. Your dentist will explain the expected timeline and next steps for restoring the tooth to full function.
Modern root canal treatment is typically no more uncomfortable than receiving a routine filling because local anesthesia numbs the area effectively before work begins. Many patients report relief from the severe pain that led them to seek care once the infected tissue is removed and the tooth is cleaned and sealed. Dental teams also use techniques to minimize discomfort during the appointment and provide clear aftercare instructions.
Some mild soreness or tenderness around the treated tooth is normal for a few days as surrounding tissues heal, and this can usually be managed with over-the-counter pain relievers as recommended. If pain increases or does not improve, contact your dental provider so they can evaluate healing and rule out complications. The goal is a smooth recovery and a comfortable outcome.
Recovery time after root canal therapy is generally short; most patients experience only mild soreness that resolves in a few days. You may feel numb for an hour or two after the appointment, so avoid chewing until sensation returns, and follow any temporary restoration care instructions to reduce the risk of damage. If antibiotics are prescribed for an active infection, take the entire course exactly as directed to support healing.
Maintain excellent oral hygiene by brushing and flossing carefully around the treated tooth, and avoid hard or sticky foods until the permanent restoration is in place. Attend follow-up visits so the dentist can confirm healing with clinical exams and radiographs and complete the protective restoration, which is essential to the tooth's long-term success. Prompt communication with your dental team helps address any concerns during recovery.
Many root canal–treated teeth benefit from a permanent restoration such as a crown to restore strength and protect against fracture. Because a treated tooth can become more brittle over time, a crown or appropriate onlay helps redistribute chewing forces and seals the tooth against recontamination. The type of restoration recommended depends on the tooth's location, remaining tooth structure, and functional demands.
Your dentist will discuss the restorative plan and timing for placing a crown or other definitive restoration so the tooth regains full function and appearance. Leaving a treated tooth without a proper permanent restoration increases the risk of breakage and may compromise the long-term outcome. Coordinating endodontic and restorative care ensures the best possible prognosis.
The primary alternative to saving a tooth with root canal therapy is extraction followed by tooth replacement options such as a dental implant, bridge, or removable partial denture. Extraction eliminates the infected tooth but introduces new considerations, including how to replace the missing tooth to preserve chewing function and prevent adjacent teeth from shifting. Each replacement option has clinical pros and cons that must be evaluated in the context of your overall oral health and preferences.
Deciding between root canal treatment and extraction involves assessing the tooth's restorability, surrounding bone support, periodontal health, and the complexity of restorative needs. A conservative, evidence-based approach favors preserving a natural tooth when a predictable, durable outcome is achievable. Your dentist will review all appropriate options and help you choose the treatment that best meets your long-term oral health goals.
With proper restoration and ongoing care, many root canal–treated teeth remain functional for decades and often for the lifetime of the patient. Long-term success depends on factors such as the quality of the root canal fill, the integrity of the final restoration, the presence of protective crown coverage when indicated, and good oral hygiene practices. Regular dental checkups and periodic radiographs help detect changes early and support lasting results.
In some cases a previously treated tooth may require retreatment or an apicoectomy if infection recurs or symptoms persist. Prompt evaluation of new symptoms or radiographic changes allows timely intervention and can often preserve the tooth. Maintaining routine dental care and addressing problems early are key to extending the service life of treated teeth.
Sedation options can help patients who experience dental anxiety or who have difficulty tolerating longer procedures by promoting relaxation and comfort. Common approaches include nitrous oxide for mild anxiety and oral or monitored sedation for deeper relaxation, depending on the patient's medical history and the procedure's complexity. The chosen method is selected to balance comfort with safety and to support a positive treatment experience.
Patients at Brian Howe DDS, Family Dentistry can discuss sedation preferences and medical considerations during the consultation so the team can recommend an appropriate plan. Pre-procedure instructions and monitoring protocols are provided to ensure safety, and your dentist will review any medical conditions or medications that may affect sedation choices. Clear communication helps tailor a care plan that keeps you calm and comfortable throughout treatment.
If you experience severe, uncontrolled pain, rapidly increasing swelling, fever, difficulty breathing or swallowing, or a spreading infection, seek immediate medical attention or emergency dental care. These signs can indicate a serious infection that may require urgent intervention to control the spread and protect your overall health. Prompt evaluation reduces the risk of complications and helps determine whether root canal therapy, drainage, or other urgent treatment is needed.
If you are able to contact your dental office, let them know your symptoms so they can advise the best next steps and arrange timely care when appropriate. If you are in Newark, Ohio and have concerns about a painful tooth outside normal office hours, proceed to the nearest emergency department or emergency dental provider without delay. Rapid assessment and treatment are important when signs of systemic involvement or severe infection are present.
Our friendly and knowledgeable team is always ready to assist you. You can reach us by phone at (740) 344-4549 or by using the convenient contact form below. If you submit the form, a member of our staff will respond within 24–48 hours.
Please do not use this form for emergencies or for appointment-related matters.
